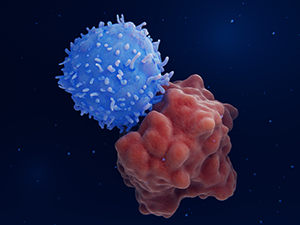
CRISPR-engineered universal T cells provide a novel approach to treating cancer
Logistics and the high cost of personalized treatment currently limit the utility of chimeric antigen receptor (CAR) T-cell therapy. Pre-manufactured universal CAR T-cell banks promise to overcome these constraints and make CAR T-cell therapy more widely accessible. To investigate the feasibility of this approach, researchers at Great Ormond Street Hospital for Children and the Great Ormond Street Institute of Child Health engineered T cells from healthy volunteers to express CAR19 in combination with several advantageous modifications. Following characterization, during a phase 1 clinical trial, the cells were administered to children with relapsed/refractory CD19-positive B-cell acute lymphoblastic leukemia (B-ALL). The results of this study, published in Science Translational Medicine, show complete remission in two out of six patients, highlighting the lifesaving potential of next-generation CAR T-cell therapies.
CAR T-cell bank production and characterization
The CAR T cells used in this phase 1 clinical trial were produced by linking CAR19 expression to the transcription activator-like effector nuclease (TALEN) mediated knockout of the T-cell receptor α chain (TRAC) and CD52. Disrupting TRAC was previously shown to help prevent graft-versus-host disease, while CD52 knockout provides a survival advantage in the presence of alemtuzumab, an anti-CD52 monoclonal antibody administered during preparative lymphodepletion. The capped, polyadenylated, and uridine-modified Cas9 mRNA used for nuclear localization was manufactured by TriLink. Characterization of the engineered cells included flow cytometric analysis of CAR19 and CD52 at day 0 and the end of production (day 12), direct sequencing of on-target editing effects, and various in vitro functional assessments to confirm CD19-specific cytotoxicity and cytokine responses.
Clinical trial results
Six patients with relapsed/refractory B-ALL, ranging from 6 months to 18 years of age, were enrolled in the trial. Eligibility was based on the presence of morphological disease (>5% blasts), a minimal residual disease of >0.01%, or exhaustion of other treatment options, including autologous CAR19 therapy. Following lymphodepletion, each patient received a single, tailored dose of the engineered CAR T cells (spanning 0.8 × 106 to 2.0 × 106/kg) before being monitored in the hospital for at least 28 days to assess toxicity and track count recovery.
Four patients had achieved sufficient remission at the end of the evaluation period to receive an allogeneic stem cell transplantation (SCT). This involved reconditioning with chemotherapy, antithymocyte globulin (a selective T-cell depleting agent), and radiotherapy prior to infusion. Of the four, two individuals relapsed after SCT, whereas two entered complete remission and remained alive and well at 3 months and 12 months post-SCT, respectively. In all cases, any complications or side effects (e.g., grade 2 cytokine release syndrome, transient neurotoxicity, skin GVHD) fell within expectations.
Extending the utility of next-generation CAR T-cell therapies
Although efforts are ongoing to improve the efficacy of pre-manufactured universal CAR T-cell banks, this study suggests they have significant potential for treating B-ALL and other types of blood cancer. Critically, their use represents a viable alternative to existing treatment regimens.
Featured service: Custom mRNA manufacturing
Article reference: Ottaviano G, Georgiadis C, Gkazi SA, et al. Phase 1 clinical trial of CRISPR-engineered CAR19 universal T cells for treatment of children with refractory B cell leukemia. Sci Transl Med. 2022; (14):668.


