mRNAs aid Natural Killer (NK) cell immunotherapy of acute myeloid leukemia (AML) in a mouse model
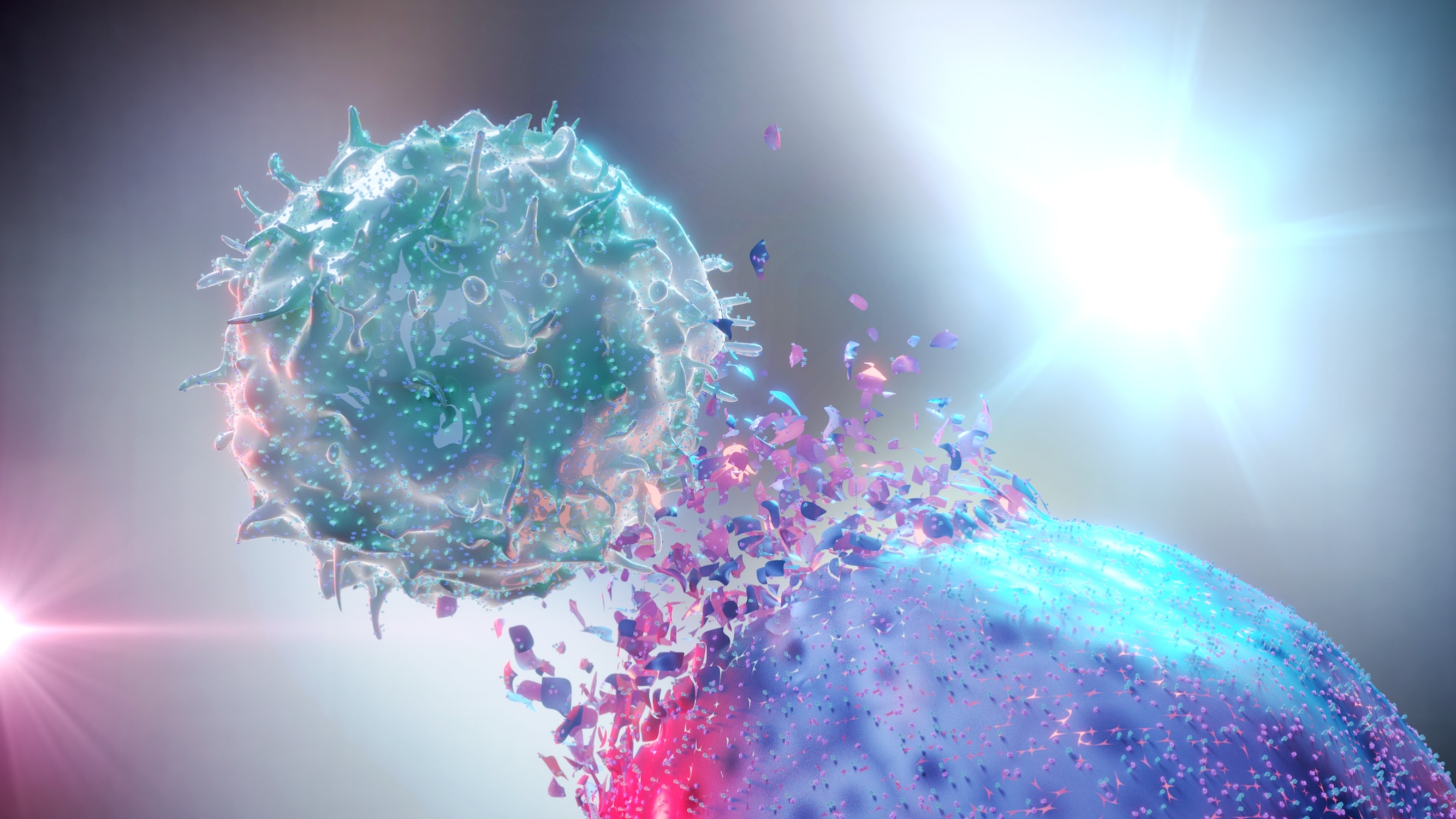
Clinical trials based on the adoptive transfer of natural killer (NK) cells have linked positive outcomes in patients with acute myeloid leukemia (AML) to the bone marrow (BM) infiltration potential of the infusion. However, researchers from the Karolinska Institute (KI) in Stockholm, Sweden, have recently discovered that AML development gradually impairs the BM homing capacity of NK cells, potentially limiting the efficacy of such treatments. Their data, published in Leukemia, show that transfecting NK cells with mRNAs coding for FUT7 and CXCR4R334X restores NK cell BM infiltration in mice with a high AML burden to nearly normal levels. This finding promises to help improve response rates for adoptive NK cell immunotherapies targeting AML and other hematological malignancies.
AML development impairs BM infiltration by infused NK cells
A xenograft AML mouse model was established by inoculating HL-60 cells into NSG-SGM3 mice and measuring human CD45 and CD33 by flow cytometry. Data demonstrated a low AML burden (2–15%) in the BM at day 18 and a high AML burden (60–80%) in the BM at day 25. When ex vivo expanded human NK cells were administered intravenously at each of these time points, flow cytometric analysis of human CD45 and CD56 in BM samples revealed a high AML burden to be associated with reduced BM infiltration.
FUT7-modified NK cells have improved BM homing in AML bearing mice
Proper fucosylation of extracellular proteins is required for NK cell binding to E-selectin on vascular surfaces. However, flow cytometric measurement of sialyl-Lewis-X (sLex) expression showed the ex vivo expanded NK cells to have low fucosylation levels. To address this, the KI researchers transiently introduced TriLink’s custom mRNA coding for FUT7 (the enzyme responsible for sLex synthesis) into the ex vivo expanded NK cells prior to infusion. This significantly improved BM infiltration in animals with a high AML burden compared to controls, which was suggested to be further enhanced by leukemia-induced up-regulation of E-selectin on BM endothelial cells.
Co-introduction of FUT7 and CXCR4R334X rewires NK cell homing in vivo
ELISA-based analysis of BM supernatants revealed that AML growth is associated with a gradual drop in levels of SDF-1α, a chemokine which exerts its effects through the CXCR4 receptor. Based on previous work in which transfection of NK cells with TriLink’s mRNA coding for CXCR4R334X (the gain-of-function variant of CXCR4) was shown to improve responses to low levels of SDF-1α, the KI researchers sought to translate this finding to the AML mouse model. This involved infusing FUT7/CXCR4R334X-modified NK cells into mice and determining the BM homing capacity by flow cytometry. Key findings included the discovery that FUT7/CXCR4R334X-modified NK cells have a significantly higher infiltration potential than unmodified control cells, and that this is comparable to infusing unmodified NK cells into healthy mice, indicating that co-introduction of FUT7 and CXCR4R334X effectively rewires NK cell homing.
Future potential
Using transient mRNA transfection to modify ex vivo expanded human NK cells prior to infusion has enhanced BM infiltration. Identifying and capitalizing on additional tumor-associated microenvironmental changes promises to improve outcomes for patients with AML and other hematologic malignancies.
Featured products: mRNA CDMO Services
Article reference: Sanz-Ortega L., Andersson A. and Carlsten M. Harnessing upregulated E-selectin while enhancing SDF-1α sensing redirects infused NK cells to the AML-perturbed bone marrow. Leukemia. Published online January 5, 2024. https://www.nature.com/articles/s41375-023-02126-1


