In Vivo Production of CAR T Cells Promises to Treat Cardiac Injury
Activation of cardiac fibroblasts in response to myocardial injury is part of the normal wound healing process. However, in many chronic heart diseases, activated fibroblasts fail to quiesce and instead continue secreting extracellular matrix, which can lead to fibrosis. Although such fibroblasts have successfully been eliminated in mice using chimeric antigen receptor (CAR) T cells, a drawback of this approach is that the engineered cells' indefinite persistence can limit any response to future injury. To address this risk, researchers at the University of Pennsylvania have developed a method for transiently producing functional antifibrotic CAR T cells in vivo using lipid nanoparticle (LNP) mRNA technology. Their results, published in Science, show this strategy to reduce fibrosis and restore cardiac function in a mouse model of heart failure.
A novel approach to CAR T cell production
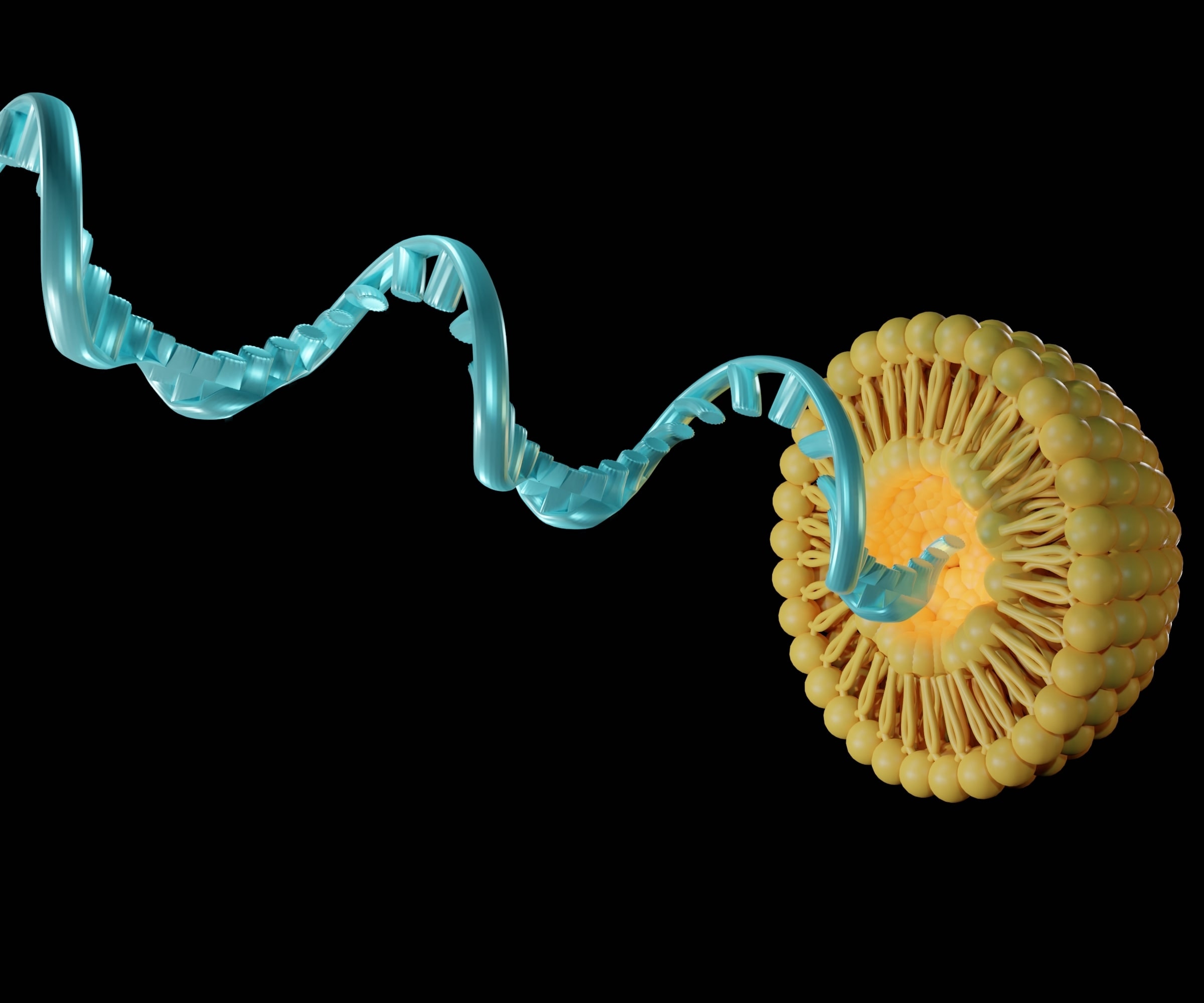
Using mRNA to produce CAR T cells avoids integration-associated safety concerns. Yet, the therapeutic utility of this method is limited by the need for repeated cycles of T cell removal and ex vivo electroporation. To determine whether LNP mRNA technology could be used to produce CAR T cells in vivo, researchers at the University of Pennsylvania synthesized mRNA encoding a CAR against fibroblast activation protein (FAP), a marker of activated fibroblasts. They packaged it into LNPs targeting CD5; a protein naturally expressed on T cells. The mRNA was stabilized by incorporating N1-Methyl-pseudouridine-5'-triphosphate into the molecular backbone and using CleanCap® reagent for co-transcriptional capping.
Highly efficient in vitro delivery
To establish proof-of-concept, CD5/LNPs containing mRNA encoding the FAP CAR (CD5/LNP-FAPCAR) were incubated with freshly isolated, activated murine T cells in vitro. Flow cytometry analysis showed >80% of cells to express the encoded protein after 48 hours, compared to just 7% of cells incubated with LNPs featuring isotype control antibodies. Critically, when the resultant FAPCAR T cells were co-incubated with FAP-expressing HEK293T cells, they were found to cause dose-dependent cell death.
Effective in vivo T cell reprogramming
The in vivo efficacy of CD5/LNP-FAPCAR was confirmed using an established murine model of cardiac injury and fibrosis. Injection of CD5/LNP-FAPCAR yielded a consistent population of FAPCAR+ T cells within 48 hours, and FAPCAR expression was lost within a week. Treated animals exhibited a statistically significant improvement in the heart-to-body weight ratio, indicative of reduced fibrosis. Analysis of cardiac function by echocardiography showed marked improvements in CD5/LNP-FAPCAR treated animals compared with the control group. These findings suggest in vivo production of CAR T cells to be a promising therapeutic strategy for translation to the clinic, not only to treat fibrosis but also to address many other conditions through engineering specific immune functions.
Featured product:: N1-Methyl-pseudouridine-5'-triphosphate and CleanCap®
Article Reference: Rurik JG, Tombácz I, Yadegari A, et al., CAR T cells produced in vivo to treat cardiac injury, Science. 2022; 375:91–96.


