Individualized self-amplifying mRNA neoantigen vaccines promise improved outcomes for cancer patients
Immunotherapies targeting the immune checkpoints cytotoxic T-lymphocyte antigen 4 and programmed death receptor 1 have revolutionized the treatment of solid tumors. However, because these checkpoint inhibitors (CPIs) mainly function by reactivating pre-existing tumor-specific T-cell responses, they offer only limited benefit to patients bearing tumors with low immune reactivity. Vaccines that expand pre-existing tumor-specific T cells and prime them de novo promise to overcome this problem but have so far seen little success. Researchers at Gritstone bio, Inc., developed a series of heterologous self-amplifying mRNA (saRNA) vaccines to address the shortcomings of evolving vaccination strategies, each based on a patient-specific neoantigen. The interim results of a phase 1 trial published in Nature Medicine showed that when this vaccine regimen was administered in combination with CPIs, it improved overall survival for patients with advanced metastatic cancers.
Vaccine design
Although human adenovirus vaccine vectors promote robust T-cell responses, the high prevalence of anti-adenoviral antibodies in human serum can limit their efficacy. To circumvent this issue, Palmer et al. created a series of vaccines comprising a chimpanzee adenoviral vector (ChAd68) and a fully synthetic Venezuelan equine encephalitis virus (VEEV) vector. By engineering each VEEV to express a saRNA for a patient-specific neoantigen, they could provide personalized therapies to the individuals enrolled in the clinical trial (NCT03639714) for delivery with nivolumab and ipilimumab. The saRNAs used in this study were manufactured by TriLink..
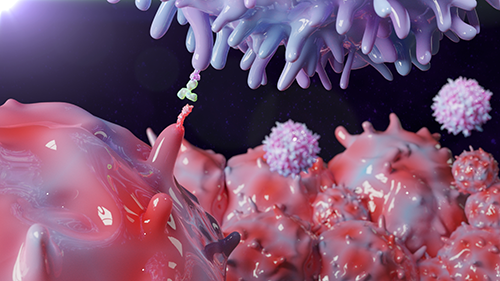
Vaccination induces neoantigen-specific CD8+ T cells
To assess vaccine immunogenicity, Palmer et al. developed a set of patient-specific minimal epitope (8–11mer) peptide pools, each designed to include the 40 highest-ranked predicted neoepitopes. These were used to stimulate patient-derived peripheral blood mononuclear cells (PBMCs), isolated following a boost vaccination. ELISpot measurement of IFN-γ responses showed vaccination-induced neoantigen-specific CD8+ T cells, a cell type critical to tumor control and clearance. These were subsequently found to kill target cells pulsed with neoantigen peptides when expanded and grown in co-culture.
T cells are increased in tumors following vaccination
For vaccine-induced T cells to exert their anti-tumor effects, they must be able to access their target cells, recognize them via the T-cell receptor (TCR), and lyse them. By performing paired TCR sequencing using tumor biopsy material, Palmer et al. showed that the same clonotypes detected in PBMC preparations were also present in the tumor tissue. In addition, analysis of transcriptional activation signatures via single-cell RNA sequencing confirmed CD8 T cells to be enriched in treated samples.
Vaccination improves overall survival
Other parameters analyzed during the phase 1 trial included measurement of circulating tumor DNA through sequencing, monitoring of changes in tumor size via imaging, and tracking of overall survival. Notably, for patients with microsatellite-stable colorectal cancer (MSS-CRC), three of seven individuals remained alive with an overall survival rate at 12 months of 42.9%, suggesting personalized self-amplifying mRNA neoantigen vaccines provide lasting benefit.
Featured service: Custom mRNA manufacturing
Article reference: Palmer CD, Rappaport AR, Davis MJ, et al. Individualized, heterologous chimpanzee adenovirus, and self-amplifying mRNA neoantigen vaccine for advanced metastatic solid tumors: phase 1 trial interim results. Nat Med. 2022;28(8):1619-1629.


