- Dementia Develops in Someone in the World Every 3 Seconds
- Nucleic Acid-Based Approaches for an Alzheimer’s Drug Are Advancing
- Ionis Pharmaceuticals is First to Begin Clinical Trials with Antisense Oligonucleotide Targeting Tau
The concept of nucleic acid-based therapeutics, as originally conceived by Paul Zamecnik, goes back to his seminal publication in 1978 that I’ve blogged about previously. However, it wasn’t until the advent of automated synthesis of various types of modified oligonucleotide analogs that this “antisense” approach to drug development achieved critical mass of sustained attention. Since then, synthetic oligonucleotides and mechanisms of interference with mRNA expression have greatly expanded to now include a diverse “armory” of alternatives to combat diseases, including:
- Antisense oligonucleotides (ASOs) that induce cleavage of mRNA by RNase H or other mechanisms
- Short-interfering RNA (siRNA) that are incorporated into RISC that cleaves mRNA
- Antagomirs that block microRNA (miR) binding to mRNA
- Aptamers that bind to target proteins as drugs, or for targeted delivery of other types of drugs
- Splice-switching oligonucleotides (SSOs) that hybridize with a pre-mRNA and disrupt normal splicing
- Recently reported RNA-guided RNA-targeted CRISPR-Cas variants that can knockdown RNA systems much more specifically than siRNA
Investigating possible NA-based approaches to currently refractory, or other so-called ‘undruggable’ diseases, has attracted much needed interest from academics and pharma researchers, as well as implementation of GMP procedures. Recognizing this need, and the absence of a conventional drug to treat Alzheimer’s disease (AD)—the leading cause of dementia in adults—kindled my efforts to research the literature and write this blog.
What is AD?
 Auguste Deter, who was a patient of German psychiatrist Alois Alzheimer, was the first described case of what became known as Alzheimer's disease. Taken from Wikipedia.org
Auguste Deter, who was a patient of German psychiatrist Alois Alzheimer, was the first described case of what became known as Alzheimer's disease. Taken from Wikipedia.org
According to a U.S. National Institutes of Aging fact sheet, AD is an irreversible, progressive brain disorder that slowly destroys memory and thinking skills, and eventually the ability to carry out the simplest tasks. In most people with AD, symptoms first appear in their mid-60s. Statistics vary, but AD accounts for as much as ~80% of all dementia—an umbrella term for loss of cognitive functioning—which will develop in someone in the world every 3 seconds, and afflict close to 50 million people in 2017. This is based on estimates by Alzheimer’s Disease International.
Brains from bodies of deceased persons who had advanced AD exhibit overall “shrinkage,” macroscopically, compared to persons who did not show indications
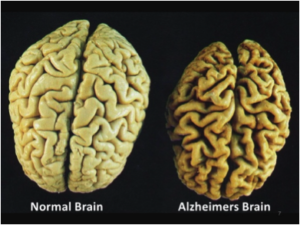 Taken from fellowshipoftheminds.com
Taken from fellowshipoftheminds.com
of AD. Microscopically, AD is characterized by accumulation of toxic “amyloid plaques,” which are sticky buildup that accumulate outside nerve cells, or neurons. Amyloid is a protein that is normally found throughout the body, but in AD the protein is cleaved by beta secretase (BACE1) and gamma secretase to yield amyloid beta (Aβ) peptides of 36–43 amino acids. Aβ molecules can aggregate to form flexible soluble oligomers that may exist in several forms. It is now believed that certain misfolded oligomers can induce other Aβ molecules to also take the misfolded oligomeric form, leading to a chain reaction akin to a prion infection.
 Amyloid plaques. Taken from slideshare.net
Amyloid plaques. Taken from slideshare.net
Since 1993, when a variant of the apolipoprotein E (APOE) gene was found to be strongly associated with increased vascular and plaque Aβ deposits in late-stage AD patients, many researchers have probed APOE connections to Aβ. However, in September 2017 this investigative field was reportedly “stunned” by results published by Shi et al. showing that neurotoxic effects associated with APOE may result from a damaging immune response to a different protein named tau, encoded by the MAPT gene. This late-breaking scientific news is part of an ongoing story of AD molecular pathology that interested readers will want to follow.

Recent Advances in Nucleic Acid-Based Drugs for AD
My strategy for researching this topic began with querying Google Scholar for “Alzheimer’s” articles since 2013 that are coupled with key words for each of the above nucleic acid-based drug modalities, namely, “antisense,” “siRNA,” etc. This led to literature ranked by Google Scholar according to citation counts. I then perused this information to select items for each of these modalities. I linked to the search results for readers interested in further digging into these topics.
A report that caught my attention was by Lane et al. from Ionis (formerly Isis) Pharmaceuticals. This company (founded and still led by Stanley Crooke, about whom I’ve blogged) is widely acknowledged to be the leader in clinical development of antisense therapeutics. In a nutshell, Lane et al. hypothesized that, given the critical role for tau (see above) in transducing Aβ-linked neurotoxicity, reducing the synthesis of tau could have a therapeutic effect.
Ionis-MAPTRx, a 2'-O-methoxyethyl chimeric ASO, was found to reduce tau expression in transgenic mice and was tested in FDA/IND-enabling toxicology studies in rodents and non-human primates (NHPs). Intrathecal administration of the highest dose in NHPs resulted in a mean MAPT mRNA reduction of 77% in frontal cortex and 74% in hippocampus without dose-limiting side effects. Following up on this, I found that on October 13, 2017, Ionis announced initiation of a Clinical Study of Ionis-MAPTRx in patients with AD, thus earning a $10 million milestone payment from Biogen.
In another ASO approach, Farr et al. have further investigated their previously reported 20-mer phosphonothioate oligonucleotide (GAO) that had been shown to knockdown levels of glycogen synthase kinase (GSK)-3β, which is a multifunctional protein implicated in the pathological characteristics of AD, including neurofibrillary tangles, Aβ, and neurodegeneration. In the present study, they assessed the impact of peripherally administered GAO on learning and memory—measured by a T-maze (see picture)—in two different mouse models of AD, as well as knockdown of protein expression. GAO-treated mice showed improved acquisition and retention, along with decreased protein levels. They concluded that this study “supports peripherally administered GAO as a viable means to mediate GSK-3β activity within the brain and a possible treatment for AD.”

To learn about a T-maze, click here.

While there are several intriguing studies of ASOs associated with AD therapy, siRNA is much more common in the research and treatment of AD. The report that I found most interesting was published by Rassu et al. in 2017, and is titled Nose-to-brain delivery of BACE1 siRNA loaded in solid lipid nanoparticles for Alzheimer’s therapy. My interest stemmed from the focus on developing delivery technology to achieve “nose-to-brain” as a very convenient, non-invasive route for delivery using solid lipid nanoparticles (SLNs), which are viewed as promising technologies for drug-delivery.
In this report, the siRNA targeted the secretase BACE1, which has been widely investigated because of its involvement in forming neurotoxic Aβ peptides, as mentioned above. To increase the transcellular pathway in neuronal cells, a short cell-penetrating peptide derived from rabies virus glycoprotein known as RVG-9R was used, based on previous studies demonstrating that intravenous treatment with an RVG-9R-bound antiviral siRNA afforded robust protection against fatal viral encephalitis in mice. Building on this prior knowledge, Rassu et al. optimized the molar ratio of RVG-9R and BACE1 siRNA, and investigated chitosan-coated and uncoated SLNs as a nasal delivery system capable of exploiting both olfactory and trigeminal nerve pathways.

The positive charges from protonated amino (NH2) groups of the coating formulation ensured muco-adhesiveness to the particles, and prolonged residence-time in the nasal cavity. They studied cellular transport of siRNA released from the SLNs using the Caco-2 cells, which is a human epithelial colorectal adenocarcinoma cell line, as a model for epithelial-like phenotypes. It was found that siRNA better permeates the monolayer when released from chitosan-coated SLNs vs. uncoated SLNs or “naked” siRNA.

MicroRNA-146a (miR-146a) is upregulated in the brains of patients with AD and induces activation of tau (see above). To determine whether reducing miR-146a could ameliorate tau-related AD pathologies, Wang et al. assessed its levels and the use of a miR-146a inhibitor (antagomir) in a validated mouse model of AD. The antagomir and solvent control were delivered into the hippocampus of these mice at three months of age and memory was tested in all mice using several types of mazes (see above) before extracting brain samples for quantitative RT-PCR using measurements of miR-146a and protein targets. In a nutshell, the overall results demonstrated that improvement of memory by intrahippocampal miR-146a antagomir was associated with the predicted alterations in the tau-related neural pathway, confirming that inhibition of miR-146a expression has a therapeutic effect in this mouse model of AD. It was concluded that “this data support (sic) the concept that miR-146a antagomir is a potential efficacious therapeutic target for the tau pathology of AD.”

In a study published by Liang et al. in 2015, systematic evolution of ligands by exponential enrichment (SELEX) with random-sequence libraries was used to obtain a DNA aptamer (A1). That aptamer is pictured below, and has been shown to have high-affinity binding to purified human BACE1 extracellular domain. They subsequently confirmed that A1 exhibited a marked inhibitory effect on BACE1 activity in an AD cell model, based on decreased concentrations of Aβ fragments and BASE1 protein. These investigators concluded that “these findings support the preliminary feasibility of an aptamer evolved from a SELEX strategy to function as a potential BACE1 inhibitor. To our knowledge, this is the first study to acquire a DNA aptamer that exhibited binding specificity to BACE1 and inhibited its activity.”
Splice-Switching Oligonucleotides
According to Hinrich et al., apolipoprotein E receptor 2 (ApoER2), which is involved in long‐term potentiation, learning, and memory, has been proposed to be involved in AD, though a role for the receptor in the disease is not clear. ApoER2 signaling requires amino acids encoded by alternatively spliced exon 19. To test the role of deregulated ApoER2 splicing in AD, they designed a splice-switching oligonucleotide (SSO) that increases exon 19 splicing. Treatment of AD mice with a single dose of SSO corrected ApoER2 splicing for up to 6 months and improved synaptic function and learning and memory. They concluded that “these results reveal an association between ApoER2 isoform expression and AD, and provide preclinical evidence for the utility of SSOs as a therapeutic approach to mitigate AD symptoms by improving ApoER2 exon 19 splicing.”
Individuals heterozygous for the Swedish mutation of the amyloid precursor protein (APPswe) display an increased β-secretase cleavage leading to higher Aβ levels—both in brain and peripheral tissues, according to Gyorgy et al. They added that the mutation is a double base change adjacent to each other and has a dominant effect, which led them to hypothesize that the CRISPR system would selectively disrupt the mutated allele without affecting the wild-type (wt) allele.
In a nutshell, human APPswe fibroblasts and non-mutated control fibroblasts from subjects of the same family were grown in vitro, and then transfected with a Cas9 plasmid together with different guide RNAs (gRNAs) designed to bind either the mutated or non-mutated site with the mutation in the gRNA recognition sequence. Sanger sequencing was performed on cells that had been successfully transfected with CRISPR plasmids, and on such cells, both the APPswe mutant and wt alleles could be disrupted with gRNAs designed against the mutated and non-mutated sites, respectively. Moreover, these effects appeared to be highly specific as assayed by deep sequencing as they did not find any random mutations on the wt allele with the gRNA targeting the mutated site or vice versa.
This study reported in 2016 was said to “[provide> the first experimental evidence that the CRISPR/Cas9 method could be used to develop a novel treatment strategy against familial forms of Alzheimer's disease caused by dominant mutations.”
Closing Comments
From the above sampling of publications reporting promising results for nucleic-acid-based therapeutic approaches to AD, I hope you will agree with me that it seems likely a clinically successful drug will prevail. What and when are uncertain, but I’m betting that something will be Ionis-MAPTRx , which is the most advanced clinical candidate to date.
Addendum

Alzheimer’s disease may move, cancer-like, from place to place in the body, lodging in the brain after originating in peripheral tissues, according to October 31, 2017 news in GEN. This cancer-like mobility was demonstrated through a technique called parabiosis—the surgical union of two specimens to allow them to share a blood supply, as shown here. This technique was used to keep pairs of mice together for several months, wherein normal mice, which don't naturally develop AD, were joined to transgenic AD mice, modified to carry a mutant human gene that produces high levels of plaque-forming Aβ. It was reported that human Aβ originating from transgenic AD mice entered the circulation and accumulated in the brains of normal mice, forming cerebral amyloid angiopathy and Aβ plaques after a 12-month period of parabiosis.






