- DIY Cholesterol and Vitamin D Monitoring Using Smartphones
- Single-molecule Microscopy on Smartphones…Coming Soon?
- Pee-powered Smartphones Developed
- Solar Powered Smartphone-assisted “sample-to-answer” with PCR and Human Skin Biopsies Demonstrated
Prologue
It’s hard to believe that the first cell phone (invented about 30 years ago) was actually considered to be very convenient even though it weighed more than two pounds and looked like a large brick—plus it took 10 hours to charge the battery to get only 30 minutes of talk-time—“o BTW no txt” back then, either! Fortunately, that cell phone has evolved into present day smartphones, which are amazingly versatile and seemingly ubiquitous extensions of our hands, thumbs, mouths, and minds that can talk to us and remind us what to do.
 Motorola produced the first handheld mobile phone (far left). Martin Cooper, a Motorola engineer and executive, made the first mobile telephone call from handheld subscriber equipment on April 3, 1973 in front of reporters, placing a call to Dr. Joel S. Engel of Bell Labs. Cooper has stated his vision for the handheld device was inspired by Captain James T. Kirk using his Communicator (far right) in the 1960s television show Star Trek.
Motorola produced the first handheld mobile phone (far left). Martin Cooper, a Motorola engineer and executive, made the first mobile telephone call from handheld subscriber equipment on April 3, 1973 in front of reporters, placing a call to Dr. Joel S. Engel of Bell Labs. Cooper has stated his vision for the handheld device was inspired by Captain James T. Kirk using his Communicator (far right) in the 1960s television show Star Trek.
Evolution of Smartphones
Present day smartphones are essentially hand-held computers with lots of processing speed and memory that allow us to communicate in various ways, take remarkably high-quality digital pictures, “surf the net”, have docking ports, and can run hundreds of thousands of applications. Given their impressive functionality and remarkable convenience, it’s not surprising that there is increasing interest in developing plug-in accessories to enable smartphones to carryout various types of bio-medical applications.
One of my previous posts highlighted a report of DNA isothermal amplification/fluorescence detection using a disposable microchip interfaced with an iPod Touch—and transmitting the results via a WiFi interface—as an example of the trend toward point-of-care (POC) and even self-diagnostic tools. Following are a few recent examples that further illustrate this trend employing smartphones.
Testing Cholesterol and Vitamin D Levels with Your Smart Phone
It is estimated that 60% of adults in the US have high cholesterol (>200 mg/dL), and 37 million have very high cholesterol (>250 mg/dL). Studies on the effect of serum cholesterol on coronary heart disease mortality indicate that there is a 17% increase in mortality for every 20 mg/dL increase above 210 mg/dL, but often time high cholesterol goes undetected.
Earlier this year, a team of US scientists reported that they had developed a smartphone accessory that will allow individuals to test their blood cholesterol levels themselves. Self-detection and routine monitoring would undoubtedly save lives given that cholesterol levels can often be controlled through simple changes in diet such as consuming less saturated fat.
 Prof. David Erickson using his iPhone interfaced with a blood test strip. Photo credit: Jason Koski/University Photography; taken from news.cornell.edu via Bing Images.
Prof. David Erickson using his iPhone interfaced with a blood test strip. Photo credit: Jason Koski/University Photography; taken from news.cornell.edu via Bing Images.
Prof. David Erickson and co-workers from Cornell University in New York developed a system that consists of a small accessory device that attaches onto a smartphone, an app, and dry reagent test strips that are already commercially available. A drop of blood is placed onto the test strip and an enzymatic, colorimetric reaction occurs. This strip is then placed into the accessory device and an image of the strip is generated using the camera on the phone. The app then quantifies the color change and converts this into a blood cholesterol concentration using a calibration curve. Check out this “must see” video of Prof. Erickson demonstrating how it all works.
According to Megan Tyler reporting in Chemistry World, the achievement of Erickson and his colleagues should not be understated. Although what they have done may sound simple, developing a smartphone-based system that enables precise and reproducible diagnostic measurements is actually very difficult. She adds that “the largest challenge comes from having to account for different lighting conditions and reaction times, differences between the cameras and camera settings in different types of phone, and the potential for misalignment of the test strip.” The team overcame the lighting problem by using the accessory device to block out external light so that the test strip would be uniformly illuminated by the flash on the camera. Meanwhile, algorithms in the app account for the other potential variables.
Tyler reports that Erickson and co-workers are now working to commercialize their system, so it may be available for the general public to purchase in the near future.
I contacted Prof. Erickson to obtain a copy of his publication about this system (called “smartCARD”—smartphone Cholesterol Application for Rapid Diagnostics) so I could read about the details.
 Read about low, normal, and high levels of HDL, LDL, triglycerides and cholesterol at Understanding Cholesterol (taken from thescienceofeating.com via Bing Images).
Read about low, normal, and high levels of HDL, LDL, triglycerides and cholesterol at Understanding Cholesterol (taken from thescienceofeating.com via Bing Images).
In that paper, he concludes by stating that “…using the smartCARD system presented here it is possible to measure other commercially available colorimetric test strips for LDL, HDL, cholesterol, and triglycerides.” Such a device would be a great advance in “cloud” based self-diagnostics and monitoring of this quartet of compounds critical to our cardiovascular health.
As I was finishing this blog, I came across yet another publication led by Prof. Erickson entitled “A smartphone platform for the quantification of vitamin D levels.” The abstract begins with pointing out that Vitamin D deficiency has been linked to a number of diseases and adverse outcomes including: osteoporosis, infections, diabetes, cardiovascular diseases, and even cancer. At present the vast majority of vitamin D testing is performed in large-scale laboratories at the request of a physician as part of an annual panel of blood tests. In contrast, Erickson and coworkers developed a DIY system for rapid quantification of vitamin D using a system similar to the cholesterol test decribed above that enables colorimetric detection of Vitamin D using a novel gold nanoparticle-based immunoassay. This system was compared with well-established ELISA test kits for serum samples of unknown concentration, and gave equivalency of the results. These investigators concluded that they “envision this as the first step towards the development of the NutriPhone, a comprehensive system for the analysis of multiple vitamins and micronutrients on a smartphone.”
Single-molecule Microscopy on a Smartphone…Coming Soon?
Lord Kelvin—17th century inventor of the eponymous Kelvin temperature scale and source of provocative quotes—helped calculate Avogadro's number, one I know all too well from my days working in the lab with seemingly very tiny quantities of material, such as picomoles of oligonucleotide primers for PCR. Looking back, the number of oligonucleotide molecules was still quite large, 6.022 x 1011, thus I’ve been mightily impressed—if not downright amazed—by the trend in new technologies for manipulating and optically detecting single molecules, let alone doing this using a smartphone!
Single-molecule optical detection on a smartphone would be truly amazing because it would need to enable technical achievements that usually require big, powerful lasers and large microscopes that take up lots of bench space and operate in a pitch-black lab. A major step toward this seemingly impossible goal has received considerable editorial praise in ACS Nano—a premier specialty journal of the American Chemical Society—as well as widespread science media coverage. The team at UCLA that’s getting all this well-deserved attention is led by Prof. Aydogan Ozcan, whom I wrote about here last year as “adapting smartphones for measurement of the cell count of HIV patients in resource limited settings or doing fluorescent microscopy.”
According to the UCLA Newsroom, your smartphone now can see what the naked eye cannot: a single virus less than one-thousandth of the width of a human hair. Prof. Ozcan’s team have created a portable smartphone attachment that can be used to perform sophisticated field testing to detect viruses and bacteria without the need for bulky and expensive microscopes and lab equipment. The device weighs less than half a pound.
"This cellphone-based imaging platform could be used for specific and sensitive detection of sub-wavelength objects, including bacteria and viruses and therefore could enable the practice of nanotechnology and biomedical testing in field settings and even in remote and resource-limited environments," Ozcan said. "These results also constitute the first time that single nanoparticles and viruses have been detected using a cellphone-based, field-portable imaging system."
The new research, published in ACS Nano, comes on the heels of Ozcan's other recent inventions, including a cellphone camera–enabled sensor for allergens in food products and a smart phone attachment that can conduct common kidney tests.
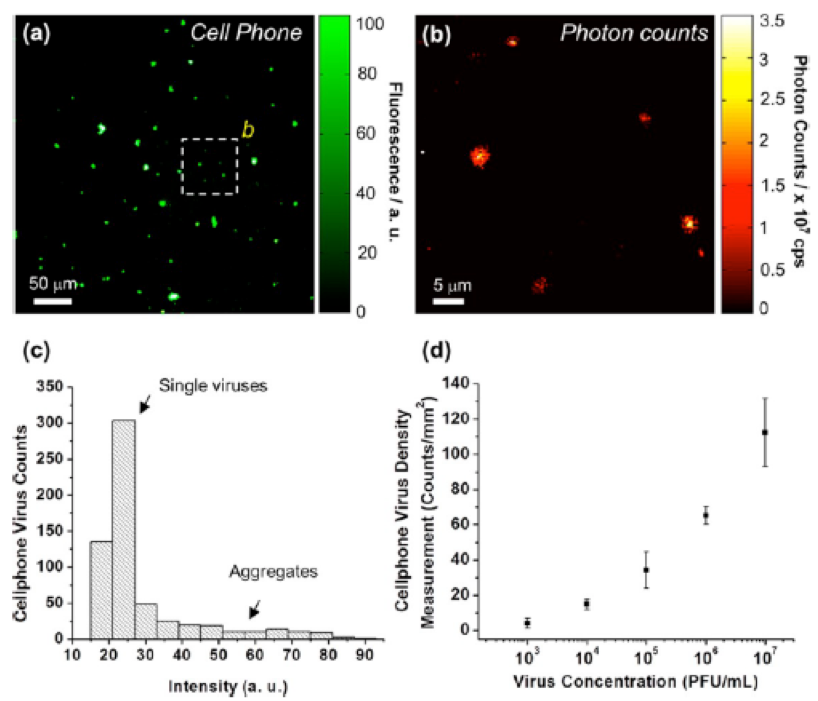
Capturing clear images of objects as tiny as a single virus is difficult because the optical signal strength and contrast are very low for objects that are smaller than the wavelength of light. In the ACS Nano paper, Ozcan details a fluorescent microscope device fabricated by 3D printing—a very hot trend in science, and consumer products—that contains a color filter, an external lens and a laser diode. As pictured here, the diode illuminates fluid or solid samples at a steep angle of roughly 75 degrees. This oblique illumination avoids detection of scattered light that would otherwise interfere with the intended fluorescent image.
Using this device attached to the camera module on a smartphone, Ozcan's team was able to detect single human cytomegalovirus (HCMV) particles. HCMV is a common virus that can cause birth defects such as deafness and brain damage. This same virus can hasten the death of adults who have received organ implants, who are infected with the HIV virus or whose immune systems have otherwise been weakened. A single HCMV particle measures about 150–300 nanometers; a human hair is roughly 100,000 nanometers thick. To verify these results, researchers in Ozcan's lab used a photon-counting confocal microscope.
.
Hopefully, Prof. Ozcan’s vision of a smartphone-based “field-portable imaging system" will become a reality in the near future. If so, this raises the challenging issue of having adequate battery power for the smartphone. Solar-based battery charging stations are one solution, but what if the sun doesn’t cooperate when needed? The next section describes an alternative approach that—in my opinion—is quite creative, to say the least.
“Pee Powered” Smartphones
As reported by Jennifer Newton in Chemistry World, the first cell phone battery to be directly charged by microbial fuel cells feeding on urine has been described by scientists in the UK. This work builds upon previous experiments in 2011 aimed at development of urine-powered fuel cells by Loannis Leropoulos and colleagues at Bristol Robotics Laboratory. They had shown that urine was an excellent fuel for direct electricity generation. As a bonus, the cells can reclaim essential nutrients from the urine, making wastewater treatment easier.

The team hopes their work will lead to emergency charging devices for remote locations. The diagram below illustrates one embodiment. Some field conditions might require alternative—dare I say primitive—means of collecting urine, as well as easily portable fuel cells.
If you’ve been exploring the diagnostic potential of smartphones or, shall we say, organic ways of powering these phones, we’d be most interested in hearing from you via the comments section below. As always, all thoughts and opinions are welcomed.
Postscript
After completing this post, Prof. Erickson’s group published a proof-of-concept study of a solar powered, smartphone-assisted “sample-to-answer” molecular diagnostic test with PCR and human skin biopsies. The following are key aspects of the abstract from Nature:
"Here we integrate solar heating with microfluidics to eliminate thermal cycling power requirements as well as create a simple device infrastructure for PCR. Tests are completed in less than 30 min, and power consumption is reduced to 80 mW, enabling a standard 5.5 Wh iPhone battery to provide 70 h of power to this system. Additionally, we demonstrate a complete sample-to-answer diagnostic strategy by analyzing human skin biopsies infected with Kaposi's Sarcoma herpesvirus through the combination of solar thermal PCR, HotSHOT DNA extraction and smartphone-based fluorescence detection. We believe that exploiting the ubiquity of solar thermal energy as demonstrated here could facilitate broad availability of nucleic acid-based diagnostics in resource-limited areas."